A comprehensive analysis across multiple ER+/HER2- breast cancer cohorts investigating genomic and transcriptomic differences between the high proliferation/low ER-related signaling (MKShi/ERSlo) subgroup and other ER+/HER2- tumors, recently published on British Journal of Cancer by researchers from Michelangelo Foundation and San Raffaele Hospital, suggests novel therapeutic strategies to improve patient survival.
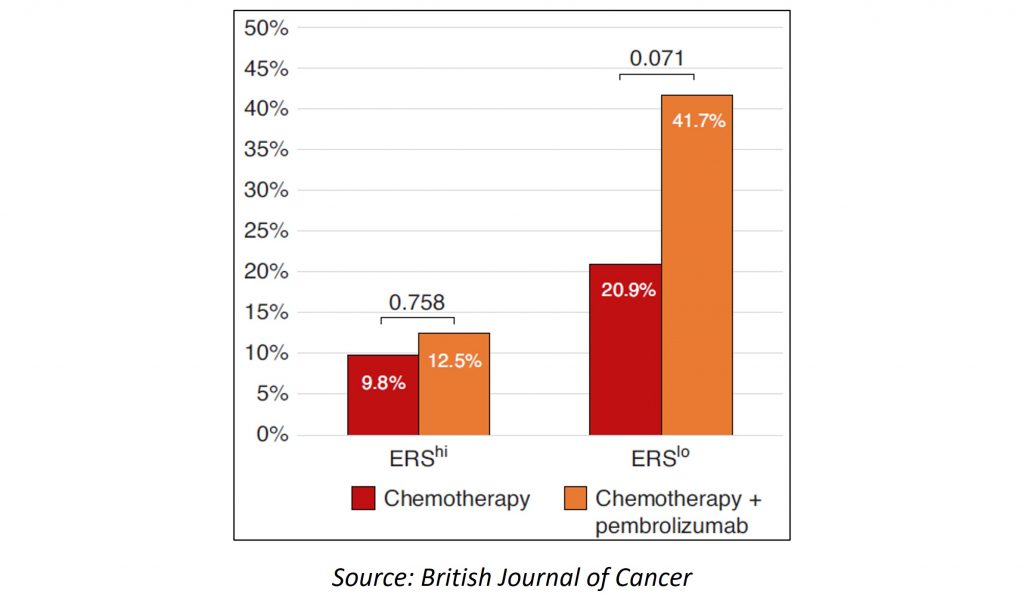
In this study, authors investigated treatment responses and molecular features in luminal MKShi/ERSlo breast cancers, analyzing gene expression data from patients who received neoadjuvant chemotherapy with or without pembrolizumab or endocrine therapy with or without palbociclib to assess treatment response by MKShi/ERSlo-subgroups. Results show that MKShi/ERSlo tumors had higher pathological response rates to neoadjuvant chemotherapy versus MKShi/ERShi tumors (22% vs 8%) but a higher recurrence risk (4-year metastases-free survival of 70% vs 94%). Other molecular features of MKShi/ERSlo tumors included TP53 and PIK3CA mutations, a high expression of biomarkers associated with palbociclib-resistance (Cyclin-E, Rbsig and IRPR) and immunotherapy-response. MKShi/ERSlo tumors retained high proliferation after endocrine therapy with or without palbociclib but had higher pathological complete response rates when pembrolizumab was added to neoadjuvant chemotherapy. Taken together, these results show that MKShi/ERSlo tumors represent a distinct molecular subset within ER+/HER2- breast cancers: they have dismal outcomes and are enriched in chemotherapy-sensitive but endocrine therapy- and palbociclib-resistant tumors. As authors conclude, «Their molecular characteristics provide an explanation for the higher rate of endocrine resistance and overall poorer prognosis. Importantly, a subset of MKShi/ERSlo tumors exhibits high chemotherapy sensitivity, as indicated by the relatively high complete pathological response rate of approximately 20%, which appears to be further improved by the addition of pembrolizumab to neoadjuvant chemotherapy. Additionally, around 30% of these cancers harbor PIK3CA mutations, suggesting that adjuvant PIK3CA inhibitors may represent a class of drugs worth investigating in prospective clinical trials. Biomarker analysis and clinical data suggest a potential role for immunotherapy in MKShi/ERSlo tumors».
A comprehensive analysis across multiple ER+/HER2- breast cancer cohorts investigating genomic and transcriptomic differences between the high proliferation/low ER-related signaling (MKShi/ERSlo) subgroup and other ER+/HER2- tumors, recently published on British Journal of Cancer by researchers from Michelangelo Foundation and San Raffaele Hospital, suggests novel therapeutic strategies to improve patient survival.
In this study, authors investigated treatment responses and molecular features in luminal MKShi/ERSlo breast cancers, analyzing gene expression data from patients who received neoadjuvant chemotherapy with or without pembrolizumab or endocrine therapy with or without palbociclib to assess treatment response by MKShi/ERSlo-subgroups. Results show that MKShi/ERSlo tumors had higher pathological response rates to neoadjuvant chemotherapy versus MKShi/ERShi tumors (22% vs 8%) but a higher recurrence risk (4-year metastases-free survival of 70% vs 94%). Other molecular features of MKShi/ERSlo tumors included TP53 and PIK3CA mutations, a high expression of biomarkers associated with palbociclib-resistance (Cyclin-E, Rbsig and IRPR) and immunotherapy-response. MKShi/ERSlo tumors retained high proliferation after endocrine therapy with or without palbociclib but had higher pathological complete response rates when pembrolizumab was added to neoadjuvant chemotherapy. Taken together, these results show that MKShi/ERSlo tumors represent a distinct molecular subset within ER+/HER2- breast cancers: they have dismal outcomes and are enriched in chemotherapy-sensitive but endocrine therapy- and palbociclib-resistant tumors. As authors conclude, «Their molecular characteristics provide an explanation for the higher rate of endocrine resistance and overall poorer prognosis. Importantly, a subset of MKShi/ERSlo tumors exhibits high chemotherapy sensitivity, as indicated by the relatively high complete pathological response rate of approximately 20%, which appears to be further improved by the addition of pembrolizumab to neoadjuvant chemotherapy. Additionally, around 30% of these cancers harbor PIK3CA mutations, suggesting that adjuvant PIK3CA inhibitors may represent a class of drugs worth investigating in prospective clinical trials. Biomarker analysis and clinical data suggest a potential role for immunotherapy in MKShi/ERSlo tumors»